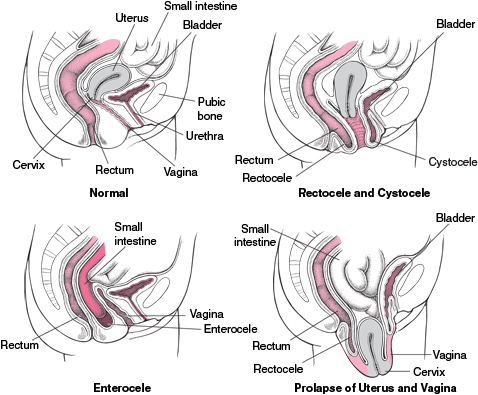
Fitting and management of Structural Pessaries for Pelvic Organ Prolapse
A Pelvic Organ Prolapse is the descent of one or more of the anterior vaginal wall, posterior vaginal wall, the uterus/cervix or the apex of the vagina (after a hysterectomy). It is estimated that 1 in 3 women are affected to the degree that the vaginal bulge extends either equal to or beyond the vaginal opening.
The 6 most common symptoms are:
Vaginal Bulge
Pelvic Pressure
Splinting/digitation
Low back ache
In severe cases bleeding, discharge and infection
Bladder and/or bowel dysfunction
Conservative management can include the use of a structural pessary. There many different types of pessaries and based on a vaginal assessment a type will be chosen that is best likely to provide the support needed for each individual situation. If fitted correctly you should not be aware of the pessary and your prolapse symptoms should be relieved.
Many pessaries can be self-managed and removed regularly however some remain in situ and are removed by your provider at a time determined by the type and how the pessary is being tolerated i.e every 4-6 months. Every 12 months it is recommended a speculum check is performed by your GP and a new pessary inserted.
If you are postmenopausal, it is recommended that you are using vaginal oestrogen supplementation prior to fitting a pessary. Your GP can prescribe this but will only do so after reviewing your medical history for any contraindications.
The process of fitting a pessary, and if indicated teaching self-management, typically requires 2-3 visits. Other conservative management strategies that are usually used in conjunction with the use of a pessary include:
pelvic floor strengthening exercises, if indicated, and managing lifestyle factors that can contribute to pelvic organ prolapse i.e. heavy lifting, constipation, respiratory conditions.
It is important to note that many women are very distressed when first experiencing pelvic organ prolapse symptoms. This is quite understandable. An important role of a pelvic floor physiotherapist is to educate and reassure you that your symptoms are in no way life-threatening and for many women can be managed well conservatively.